Mariano de Prado,1 Pedro-Luis Ripoll,2
Pau Golanó,3 Javier Vaquero,4
Nicola Maffulli 1
1 Department of Orthopaedics, Hospital USP San Carlos, Murcia;
2 Department of Anatomy, University of Barcelona;
3 Hospital Gregorio Marañon, Orthopaedic Surgery Department, Madrid, Spain;
4 Centre for Sports and Exercise Medicine, Barts and The London School of Medicine and Dentistry, Mile End Hospital, London, UK
Abstract
Several surgical options have been described to manage persistent dorsiflexion contracture at the metatarsophalangeal joint and plantarflexion contracture at the proximal interphalangeal joint of the fifth toe. We describe a minimally invasive technique for the management of this deformity. We perform a plantar closing wedge osteotomy of the 5th toe at the base of its proximal phalanx associated with a lateral condylectomy of the head of the proximal phalanx and at the base of the middle phalanx. Lastly, a complete tenotomy of the deep and superficial flexor tendons and of the tendon of the extensor digitorum longus is undertaken. Correction of cock-up fifth toe deformity is achieved using a minimally invasive approach.
Introduction
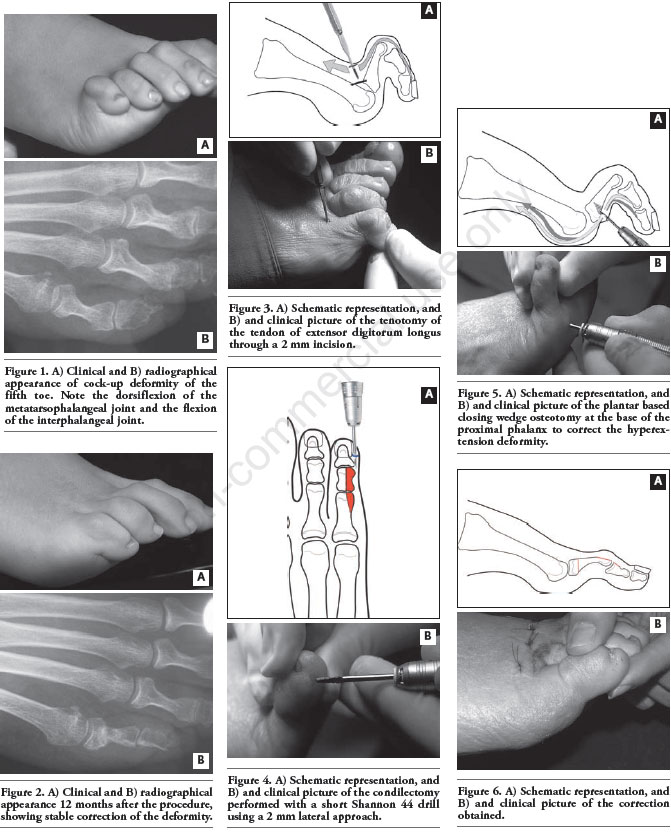
Persistent dorsiflexion contracture at the metatarsophalangeal joint and plantarflexion contracture at the proximal interphalangeal joint of the fifth toe (Figures 1A and 1B) is frequently associated with a painful hyperkeratosis1.
Surgical management is indicated in patients with marked rigidity and pain, following failure of conservative management with appropriate orthoses and shoes with a wide toe box.
Several surgical options have been described, with no clear evidence of superiority of one over another. Possible complications of surgery are iatrogenic bunionette, a floppy toe, extensive shortening of the 5th toe and subsequent hammertoe deformity of the 4th toe. Therefore, patients should be informed of the possible cosmetic and functional limitation of such procedures. In addition, some techniques involve the excision of an elliptical portion of the plantar skin is excised, a possible cause of vascular impairment of the fifth toe and hypertrophic scarring. 2,3
Some minimally invasive procedures have been proposed,4-6 but they often produce insufficient correction of the deformity. We describe a modification of the procedure described by Augustine and Jacobs4 to correct this deformity of the 5th toe. This technique consists of a plantar closing wedge osteotomy of the 5th toe at the base of its proximal phalanx associated with an exostosectomy of the head of the proximal phalanx and at the base of the middle phalanx. Lastly, a complete tenotomy of the deep and superficial flexor tendons and of the tendon of the extensor digitorum longus is undertaken.
In this way, correction of the deformity is achieved without interfering with the joint surface and producing only minimal shortening of the 5th toe, and no vascular or skin compromise (Figures 2A and 2B).
Surgical technique
The subjects operated with this technique have given written informed consent for operation and for their radiographs and clinical pictures to be taken and reproduced in print. The present study has been approved by our institutional review board.
Instrumentation/Tools
Basic surgical instruments for percutaneous foot surgery should be available: i) Scalpel Beaver handles with # 64 MIS blade (R. Beaver Inc, Waltham, Masachussetts); ii) Micro power instrument for foot-surgery (Osada Drill, Osada Electric, Co., Ltd., Tokyo, Japan); iii) Burs Shannon 44 Short (United American Medical Inc., Mc Minnville, Tennessee); iv) Small surgical rasp.
Technique
The procedure can be performed under regional nerve bloc either at the level of the ankle or of the 5th metatarsal. The patient is supine with the foot to be operated overhanging the end of the operating table. It is not necessary to use a tourniquet.
Tenotomy of the tendon of extensor digitorum longus to the 5th toe
A 2 mm incision is performed just above the extensor tendon and parallel to it at the level of the metatarsophalangeal joint. The patient is then asked to extend the 5th toe, allowing to better locate the tendon, which is fully tenotomised (Figures 3A and 3B).
Dorsal metatarsophalangeal capsulotomy
In patients with severe rigidity, capsulotomy of the metatarsophalangeal joint is performed, releasing only the superior portion of the capsule and the extensor sling. Correction of the hyperextension is remarkable.
Lateral condylectomy
If the hyper-flexion of the interphalangeal joints is difficult to correct, there often is an exostosis at the lateral condyle of the proximal phalanx of the 5th toes and at the base of the middle phalanx. If this is the case, a lateral condylectomy is indicated. A 2 mm incision is made over the dorso-lateral aspect of the 5th toe. The blade is introduced until it touches the underlying bone. The periosteum is detached from the bone with a rasp, and the exostosis is removed with the short Shannon 44 burr (Figures 4A and 4B) at slow speed with gentle oscillating movements.
Tenotomy of the flexor tendons
A 2 mm incision is performed just proximal to the plantar fold of the toe, just medial to the toe itself. The surgeon extends the 5th toe to tense the flexor tendon, which is severed with the tip of the scalpel. It should then be possible to appreciate the loss of resistance to extension in the proximal and distal interphalangeal joints.
Osteotomy of the proximal phalanx
A rasp is introduced through the same incision used for the tenotomy of the flexor tendons, and the periosteum is detached from the lateral aspect of the phalanx. A plantar based closing wedge osteotomy is performed (Figures 5A and 5B) using the short Shannon 44 burr. Complete correction of deformity is thereby achieved (Figures 6A and 6B).
Post operative care
The skin is sutured using a 4.0 monofilament suture. A bandage is put in place placing a strip of gauze to keep the proximal phalanx of the 5th toe in flexion. Another strip of gauze is applied to keep the interphalangeal joint in extension. Both dressings are joined by a bandage placed behind the interdigital pleats acting as a metatarsal spacer. Immediate mobilisation is encouraged, wearing an orthopaedic shoe for seven days, when the stitches are removed and an adhesive bandage put in place, taking care to keep the deformity reduced. Patients are taught how to change the bandage, and told to change it every day after washing the foot for the following six weeks. Around that time, complete consolidation of the osteotomies is achieved and the use of comfortable footwear is recommended.
References
1. Coughlin MJ. Lesser toe abnormalities. Instr Course Lect 2003;52:421-44.
2. Dyal CM, Davis WH, Thompson FM, Elonar SK. Clinical evaluation of the Ruiz-Mora procedure: long-term follow-up. Foot Ankle Int 1997;18:94-7.
3. Janecki CJ, Wilde AH. Results of phalangectomy of the fifth toe for hammertoe. The Ruiz-Mora procedure. J Bone Joint Surg Am 1976;58:1005-7.
4. Augustine DF, Jacobs JF. Restoration of toe function with minimal traumatic procedures including advanced diaphysectomy. Clin Podiatry 1985;2:457-70.
5. De Prado M. Cirugía percutánea del pie: técnicas quirúrgicas, indicaciones, bases anatómicas. Barcelona: Mason Publishers; 2003. pp. 1-529.
6. Roven MD. Phalangeal set. Clin Podiatry 1985;2:483-9.
Correspondence: Nicola Maffulli, Centre for Sports and Exercise Medicine, Barts and The London School of Medicine and Dentistry, Mile End Hospital, 275 Bancroft Road, London E1 4DG,England, UK.
Tel. +44.208.223.8839 - Fax: +44.208.223.8930
E-mail: n.maffulli@qmul.ac.uk
Key words: lesser toe abnormalities, osteotomy, fifth toe, minimally invasive surgery.
Received for publication: 16 June 2011.
Accepted for publication: 21 October 2011.
This work is licensed under a Creative Commons Attribution NonCommercial 3.0 License (CC BYNC 3.0).
©Copyright M. de Prado et al., 2011
Licensee PAGEPress, Italy
Surgical Techniques Development 2011; 1:e27doi:10.4081/std.2011.e27
Ver PDF